Involvement of Chemokine Receptors in Breast Cancer Metastasis Review
- Enquiry
- Open Access
- Published:
Correlation effect of EGFR and CXCR4 and CCR7 chemokine receptors in predicting breast cancer metastasis and prognosis
Periodical of Experimental & Clinical Cancer Research book 29, Article number:sixteen (2010) Cite this article
Abstract
Background
The chemokine receptors CXCR4 and CCR7 play an important part in cancer invasion and metastasis. This written report investigated the expression of CXCR4, CCR7, CXCL12, CCL21, and EGFR to illustrate the part of these biomarkers in breast cancer metastasis and prognosis.
Methods
The CXCR4, CCR7, CXCL12, CCL21, and EGFR biomarkers were analyzed along with ER, PR, and HER-2/neu in chest cancer tissue microarray (TMA) specimens, including 200 primary breast cancer specimens by immunohistochemistry. Corresponding lymph nodes from the same patients were also examined using the same method.
Results
Together with their CXCL12 and CCL21 ligands, CXCR4 and CCR7 were significantly highly expressed in tumor cells with lymph node (LN) metastasis. Similarly, EGFR was expressed highly in tumors with LN metastasis. The ligands were especially expressed in metastatic tumors than in primary tumors from the same patients. Moreover, the expression of both CXCR4 accompanied by CCR7 and CXCL12 accompanied by CCL21 were upwards-regulated. Kaplan-Meier survival analysis revealed that patients exhibiting high CXCR4, CCR7, and EGFR expression experienced a shorter survival period compared with those with low expression.
Conclusions
The expression of CXCR4, CCR7, and EGFR may exist associated with LN metastasis. Moreover, the expression of these receptors tin can serve as an indicator of undesirable prognosis in patients with breast cancer.
Background
Breast cancer ranks amongst the virtually common malignant tumors afflicting women worldwide. Despite decreased mortality rates resulting from combined therapy, breast cancer remains a leading crusade of cancer death in women. Especially in the final two decades, incidence and bloodshed rates of chest cancer have climbed sharply in China, thus attracting increased attention from researchers.
Metastasis is one feature of malignant tumors which determines the form of therapy and cancer prognosis. It is a multifactorial, nonrandom, and sequential process with an organ-selective feature. In essence, axillary lymph node metastasis is the most frequently occurring metastatic illness; it can be seen as a surrogate for distant metastasis and long-term survival [1].
Although several molecules are involved in breast cancer metastasis, precise mechanism of tumor jail cell migration to specific organs remains to be established [two]. Previously, the "seed and soil" theory was employed to explain directional metastasis, considering that certain metastasis organs possess the congenial environment of the main organ [three]. More recently, a "chemokine-receptor" model has been proposed to explain the homing of tumor cells to specific organs [4]. Chemokines belong to a super-family of modest, cytokine-like proteins that induce cytoskeletal rearrangement and adhesion to endothelial and directional migration through their interaction with G-protein-coupled receptors [ii, five].
Among the chemokines, the most interesting chemokine-receptor pair is the CXC chemokine receptor-four (CXCR4) and its lone ligand, CXC chemokine ligand-12 (CXCL12). Muller demonstrated that CXCR4 is consistently expressed in human breast cancer cells, malignant breast tumor and metastasis tumors, while its ligand CXCL12 is preferentially expressed in the lungs, liver, os marrow, and lymph nodes [2]. Thus, it can exist deduced that the CXCL12-CXCR4 axis may be associated with the metastasis of breast cancer cells to the lungs, liver, bone, and lymph nodes. Different CXCL12, however, CC chemokine ligand-21 (CCL21) - the ligand for CC chemokine receptor-seven (CCR7) - is highly expressed in the lymph nodes of chest cancer patients [5]. Thus, the CCR7-CCL21 axis can be said to assume an important role in lymph node metastasis [6]. In this study, the expression of both CXCR4 and CCR7 is combined to evaluate their contribution in the lymph node metastasis of breast cancer. The importance of growth factors such every bit epidermal growth gene receptor (EGFR) and human epidermal growth gene receptor2 (HER-2/neu) has been established in the prognosis of chest cancer. Recently, several studies take revealed the crosstalk between CXCR4 and EGFR or HER-ii/neu through transactivation by the CXCL12-CXCR4 axis.
This study aims to verify the significance of CXCR4, CCR7 and their CXCL12 and CCL21 ligands, together with EGFR in the evaluation of metastasis and the prognosis of breast cancer.
Methods
Patient selection and clinical data
The study group was equanimous of 200 specimens selected from 284 cases (84 cases were excluded owing to the absence of follow-up status) of female master invasive duct breast cancer cases diagnosed betwixt January 1997 and December 2004 at the General Hospital of Tianjin Medical Academy. Patients' records were retrieved and clinical information, histopathological record, and treatment data were all reviewed. All patients had not been subjected to chemotherapy and radiotherapy prior to surgical resection but had received chemotherapy following surgical operation. Follow-upwards information from all the patients were obtained by the authors themselves in August 2009 through visits or phone interviews with either the patients or their relatives. Mean follow-upward fourth dimension was 88 months, ranging from v to 150 months. Formalin-stock-still alkane series-embedded tumor materials and their lymph node tissues were acquired from the Department of Pathology of Tianjin Medical University'southward General Hospital. Tumor diameter, pathologic stage, and nodal status were selected from the primary pathology reports. All slides were reviewed by two pathologists to ascertain histological types and grades.
Construction of tissue microarray
Tissue microarray (TMA) blocks were constructed from formalin-stock-still, paraffin-embedded breast cancer samples stored at the Department of Pathology of Tianjin General Hospital. These TMA blocks were composed of 200 paired samples (primary tumors and corresponding lymph nodes, either metastatic or non-metastatic). Haematoxylin and eosin stained slides were reviewed to confirm the diagnosis of invasive chest cancer; later on, ii representative tumor regions were selected and marked on the donor blocks.
Tumor TMA blocks were created by punching a cylinder using a hollow needle with a diameter of two mm; the blocks were obtained from the two selected areas of each donor block earlier existence inserted into an empty alkane series cake. Subsequently, these blocks were cut into 4 μm thick slides and prepared for immunohistochemical (IHC) analysis.
Immunohistochemical assay
Using IHC staining, the expression of different proteins in human breast cancer was verified. In this process, sections were deparaffinaged in xylene prior to rehydration using gradient alcohol. Endogenous peroxydase activity was blocked by 3% hydrogen peroxide in 50% methanol for 20 minutes. For antigen retrieval, sections were treated with citrate buffer saline (pH 6.0) for fifteen minutes at 95°C in a microwave oven. After blocking with 10% normal caprine animal serum for 30 minutes at room temperature, sections were incubated with primary antibodies for another 30 minutes at room temperature. The sections were later incubated for 16 hours at 4°C. Primary antibodies and dilution were as follows: rabbit polyclonal anti-CXCR4 (Abcam, dilution 1:100); rabbit polyclonal anti-CCR7 (Abcam, dilution 1:100); rabbit polyclonal anti-CXCL12 (Abcam, dilution1:100); caprine animal polyclonal anti-CCL21 (Santa Cruz Biotechnology, dilution 1:l); rabbit polyclonal anti-EGFR (Santa Cruz Biotechnology, dilution 1:100); mouse monoclonal anti-ER (Zhongshan; gear up-to-use); rabbit polyclonal anti-PR (Santa Cruz Biotechnology, dilution 1:100); and mouse monoclonal anti-HER2 (Zhongshan; fix-to-use).
Following incubation, sections were lavaged with phosphate buffered solution (PBS) and incubated with horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG, goat anti-mouse IgG, or rabbit anti-goat IgG for 40 min at room temperature. Staining was performed using three,iii'-diaminobenzidine (DAB). Sections were counterstained with haematoxylin followed past dehydration and mounting. Negative controls were prepared using PBS in lieu of the first antibody.
Scoring of immunostaining
Sections were read by two separate pathologists blinded to patients' clinical pathology parameters. Both intensity and percentage of positive cells were considered. Five microscopy fields were reviewed in each core with 400× magnification, after which positive cells of 100 tumor cells in each field were counted. In staining for CXCR4, CCR7, CXCL12, CCL21 and EGFR, tumor cells with dark-brown cytoplasm and/or nucleus or membrane were considered positive and then scored based on four classes: none (0); weak brown (ane+); moderate dark-brown (2+); and strong brown (3+). Percentage of stained tumor cells was categorized into five classes: 0 for negative cells, 1 for 1-25%; ii for 25-50%; 3 for 50-75%; and four for >75%. Multiplication (staining index) of intensity and percentage scores was utilized to determine the result.
A staining alphabetize of ≥half-dozen was defined equally high expression, while <six was defined as low expression [seven]. On the another hand, HER2/neu was evaluated every bit positive when over 10% of tumor cells exhibited stained consecutive membranes. Unified standards were employed when evaluating estrogen receptors (ERs) and Progesterone receptors (PRs) that exceeded 10% of tumor cells, as shown in the stained nucleus.
Statistical assay
Analyses were performed using the SPSS 17.0 software package (Chicago, IL, USA). The relation betwixt CXCR4, CCR7, EGFR, and clinicopathologic characteristics were tested via Pearson χ2 analysis. The aforementioned method was employed to exam associations between these biomarkers and biologic-prognostic characteristics, such as ER, PR, and HER-2/neu expression. Correlations betwixt 2 variables were evaluated by Spearman'south rank correlation test. P-values < 0.05 were deemed statistically pregnant. Overall survival (OS) was estimated through the Kaplan-Meier method and was compared betwixt groups through the log-rank examination.
Results
Characteristics of patients and expression of biomarkers in principal tumors
Patient and primary tumor characteristics are presented in Table 1. Samples included 200 patients, among which 100 developed lymph node metastasis while 100 did non. Median age was determined at 51 years (37-74). Thirty-nine patients (xix.5%) were diagnosed with stage I cancer, 138 (69%) with stage II, 20 (10%) with stage 3, and three (1.5%) with stage IV.
In IHC staining, 77% of tumor cells were CXCR4 positive in the cytoplasm, including loftier and depression CXCR4 expression (Effigy 1A2). Meanwhile, 73% were positive in the nucleus (Figure 1A2). The amounts of CCR7 (Figure 1B2) and EGFR (Effigy 1E2) were detected in 82% and 66% of tumor cells, respectively, in the cytoplasm and/or membrane. Furthermore, 50% of ER, 49.5% of PR, and 23.5% of HER-2/neu were observed to be positive.

IHC staining for biomarkers. IHC staining for CXCR4, CXCL12, CCR7, CCL21 and EGFR. PT pertains to primary tumor, while LNMT stands for lymph node metastasis tumor. Rows correspond to the designated chemokine or receptor. The first cavalcade represents staining of negative expression in primary breast cancer with the indicated antibody. The second column indicates positive expression in main chest cancer, and the third cavalcade shows positive expression in lymph node metastasis cancer. Both PT and LNMT columns in each row are obtained from the same patient while the negative column is not. In the CXCR4 row, A2 and A3 exhibit high expression in both cytoplasm and nucleus. CCR7, CXCL12, and CCL21 all exhibit positive reaction in the cytoplasm. In the EGFR row, E2 and E3 bespeak that EGFR is expressed mainly in the membrane. Yet, a number of tumor cells announced to be positive in the cytoplasm likewise (Panels A-E, ×200).
Association of CXCR4, CCR7, and EGFR with lymph node metastasis
The immunoreactivity of CXCR4 was observed in the cytoplasm and/or nucleus of tumor cells. Cytoplasmic reactivity of CXCR4 correlated positively with lymph node metastasis of chest cancer (P < 0.001), but not with the amount of involved lymph nodes. Nuclear reactivity was not observed to exist correlated with whatever pathologic parameters. Meanwhile, CCR7 was positively expressed in the cytoplasm, and the activity was significantly correlated with lymph node metastasis (P < 0.001). Similarly, associations among the lymph node status, histological grade, and EGFR expression were observed in this study (Tabular array 1).
To verify the important effect of CXCR4 and CCR7 in metastasis, CXCR4, CCR7, and EGFR expression in primary chest cancer were compared with that in lymph node metastasis tumor. It was observed that CXCR4 and CCR7 expression in metastasis tumor was even higher, although no meaning distinction was evident. More chiefly, their respective ligands, CXCL12 and CCL21, exhibited meaning differences in expression between primary tumor and lymph node metastasis tumor (P = 0.016 and P = 0.004; Table two). Distinction between chemokines and their receptors with regard to distribution may be associated with the mechanism of metastasis; specifically, chemokines attract their receptors to certain sites along the chemokine concentration gradient.
Correlation between CXCR4, CCR7, EGFR and HER-2/neu
Although neither ER nor PR positivity was associated with degree of the biomarkers, HER2 over-expression was correlated with CXCR4 cytoplasmic positivity (p = 0.039; Table 1). As indicated by reports, the expression rate of HER2/nu in breast cancer is approximately 25%. In the results of this study, the expression of HER2 was well-nigh 20%, and amidst CXCR4 cytoplasmic positive patients, approximately 40% were associated with HER2 expression. In summary, tumors positive for CXCR4 cytoplasmic staining are more likely to be positive for HER2 over-expression.
As an contained prognostic factor for breast cancer patients, EGFR is associated with a number of pathological characteristics of chest cancer. According to the results, EGFR expression is correlated with lymph node metastasis and histological form (Table 1). Interestingly, during assay, it was discovered that close to lxx% of patients with high EGFR expression were CXCR4 and CCR7 positive as well. Spearmam'south rank correlation assay revealed that EGFR expression was significantly associated with CXCR4 cytoplasmic positivity and high CCR7 expression (P < 0.01; Table iii).
Cyclopedia of CXCR4, CXCL12, CCR7, and CCL21 expression
Later performing IHC staining for the 2 CXCL12 and CCL21 chemokines, information technology was revealed that these were correlated with i another (P = 0.017, Table iv), indicating a trend towards co-expression of these molecules in tumors. Hence, the expression of their receptors, CXCR4 and CCR7 was probable to exist tightly linked (P = .008; Tabular array 4). No significant clan was present between the expression of CXCR4 and CXCL12, nor between CCR7 and its chemokine ligand CCL21 (Table 4).
CXCR4, CCR7, and EGFR demonstrate poor prognosis past survival analysis
Follow-up investigation revealed that the median survival time was 88 months (ranging from v-150 months), within which 45 patients (22.five%) died considering of breast cancer including 28 (28%) in the tumor with metastasis group and 17 (17%) in the non-metastasis grouping. Kaplan-Meier analysis revealed that patients suffering from high levels of CXCR4 expression- either in the cytoplasm or in the nucleus -had significantly lower Os compared with those with low CXCR4 expression (P = 0.011, Figure ii; P = 0.003, Figure 3). Similarly, high levels of CCR7 and EGFR expression revealed poor prognosis (P = 0.044, Figure 4; P = 0.007, Figure five).
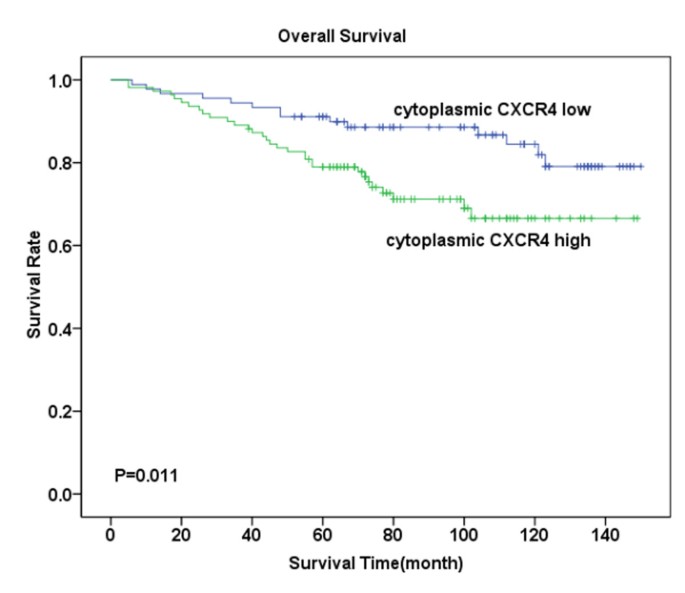
Overall survival assay for CXCR4 cytoplasmic expression. Kaplan-Meier curves for overall survival (Os) in 110 patients with high expression of CXCR4 and 90 patients with low expression of CXCR4 in cytoplasm. Survival fourth dimension sharply decreased in patients with high CXCR4 cytoplasmic expression, especially in the starting time five years, Meanwhile, survival of patients with low CXCR4 expression was merely moderately afflicted (P = 0.011).
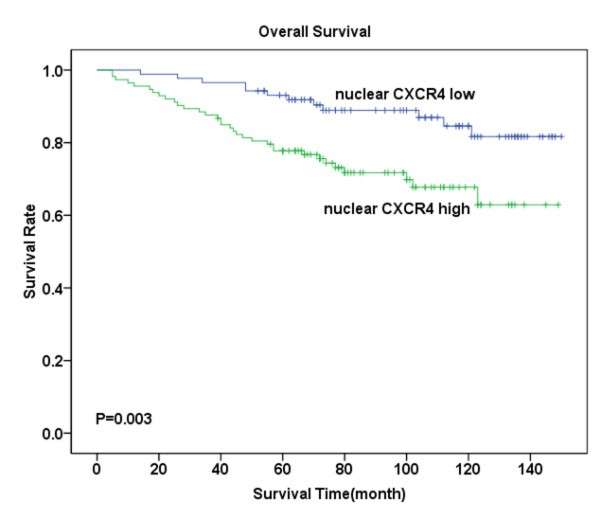
Overall survival analysis for CXCR4 nuclear expression. Kaplan-Meier curves for overall survival (OS) in 113 patients With loftier CXCR4 expression and 87 patients with depression CXCR4 expression in the nucleus. Survival time sharply decreased in patients with high CXCR4 nuclear expression, specially in the offset five years, when significantly compared with those exhibiting depression expression (P = 0.003).
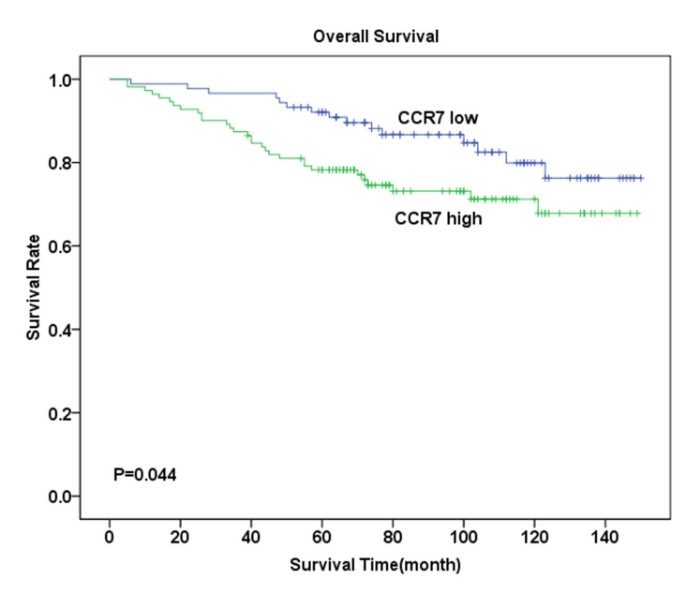
Overall survival analysis for CCR7 expression. Kaplan-Meier curves for overall survival (Os) in 111 patients with loftier CCR7 expression and 89 patients with low CCR7 expression in the cytoplasm. The divergence between these ii groups is not highly pregnant as determined past the log-rank exam (P = 0.044). However, it can be observed from the curve that in the first five years, survival charge per unit sharply decreased in patients with high CCR7 expression in the cytoplasm, while inappreciably whatsoever patient in the low expression group died during the showtime five years.
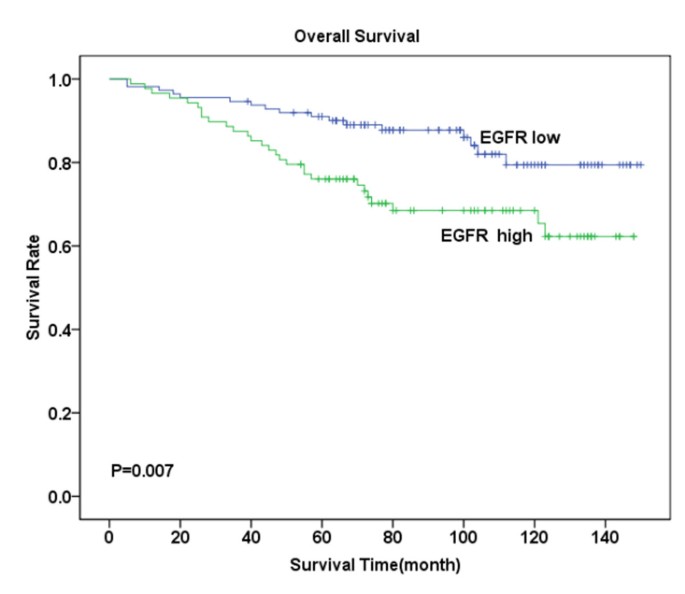
Overall survival analysis for EGFR expression. Kaplan-Meier curves for overall survival (OS) in 88 patient with high EGFR expression and 112 patients with low EGFR expression in the membrane and cytoplasm. Survival rate of patients with loftier EGFR expression was significantly low compared with those exhibiting low expression (P = 0.007).
Discussion
Recently, reports have demonstrated that chemokines and their receptors play critical roles in the development of cancer, including tumor cell growth, migration, and angiogenesis. Further, they influence the infiltration of allowed cells in a tumor [8, 9]. The mechanism of chemokines in malignant tumor metastasis may be reflected past the production of chemokine receptors by tumor cells, which answer to their homologous ligands (produced past certain organs) and drift along the chemokine gradients to trigger specific organ metastasis [10]. Out of all the known chemokine receptors, breast cancer cells specifically limited active CXCR4 and CCR7, the ligands of which are HCXCL12 and CCL21, respectively [2].
This study investigated a series of matched main and lymph node metastasis breast cancer tumors to demonstrate whether the expression of the CXCR4 and CCR7 chemokine receptors, along with expression of EGFR, predicts increased run a risk of metastasis and mortality. Present data are consistent with those in previous reports describing a positive correlation betwixt CXCR4 expression and lymph node metastasis in cases of non-pocket-sized-cell lung cancer (NSCLC), nasopharyngeal cancer, colorectal cancer, and esophageal cancer [11–fourteen]. Positive correlation has as well been reported betwixt CCR7 expression and lymph node metastasis in cases of NSCLC, breast, gastric, colorectal, esophageal, and thyroid cancer [15–xx].
It has been demonstrated that the CXCR4/CXCL12 axis as well induces chemotaxis and breast cancer cell migration. Since Muller reported that CXCR4-CXCL12 interaction governed the design of breast cancer metastasis in a mouse model, subsequent studies have been conducted in different tumors [two]. I study determined that the CXCR4 expression design correlated significantly with the degree of lymph node metastasis by investigating CXCR4 expression in 79 cases of invasive duct cancer (IDC) [21]. Su examined 85 cases of early on breast carcinoma and learned that high cytoplasmic expression of CXCR4 is associated with axillary nodal metastasis [22]. In the prent study, CXCR4 was found to be present in both cytoplasm and nucleus of tumor cells, and cytoplasmic expression was associated with lymph node metastasis. This outcome is similar to that of certain studies [22–25], merely is contrary to a scattering of reports [26]. Further, CXC chemokine 12 (CXCL12, likewise known as stromal cell derived cistron-1α, or SDF-1α) is expressed in the liver, lungs, brain, bone, and lymph nodes. on the other hand, CXCR4 is a membrane-jump G-poly peptide-coupled receptor which, together with its ligand CXCL12, mediates inflammatory and tumor jail cell migration [27]. One study has too observed CXCR4 localization at the cytoplasm in leukocyte prison cell lines with enforced CXCR4 expression and CXCL12-induced polarization of CXCR4 to the border of migrating leukocyte cells [25]. Hence, with regard to the upshot of CXCL12, CXCR4 reactivity in the cytoplasm may reflect receptor internalization. This may exist viewed as an activation land of CXCR4. Through immunohistochemistry, CXCL12 poly peptide in the cytoplasm of tumor cells was located as well, and CXCL12 expression was observed to exist higher in lymph node metastasis tumors than in primary tumors. This distinction in expression sites between chemokines and their receptors illustrates that CXCL12 attracts CXCR4 to certain metastatic sites along the concentration gradient.
Although nuclear CXCR4 is expressed in cancer cells, its role remains unclear. Spano demonstrated that nuclear CXCR4 expression represents a better issue in patients afflicted with non-pocket-sized-jail cell lung cancer [28]. All the same, in the nowadays study, later on over 10 years of follow-up observation conducted among 200 chest cancer patients, it was noted that loftier expression of both cytoplasmic and nucleus CXCR4 often indicated worse prognosis. Different localization patterns of chemokine receptors-whether nuclear or cytoplasmic-may have different levels of biological significance in cancer cells.
Similarly, the interaction betwixt CCL21 and its CCR7 receptor plays a crucial role in lymphocytes homing to secondary lymphoid organs through lymphatic vessels. A written report indicates that the hindrance of T cells homing to secondary lymphoid organs occurs because of the loss of CCL21 or the deletion of the CCR7 gene [29]. Hence, it is likely that the mechanism of CCL21 mediating migration of tumor cells to lymph nodes from primary site arising from its attraction to CCR7, which is highly expressed by primary tumors, is similar to the mechanism of the lymphocytes' homing effect. Results of this study revealed that 70% of primary breast cancer tissues and 77% of metastasis cancer cells in lymph nodes expressed CCR7. Further, at that place was a significant correlation betwixt CCR7 expression and lymph node metastasis (p < 0.001); CCL21 was especially highly expressed in lymph nodes metastasis tumor cells (68%), which was not the case in primary tumor cells (P = 0.004).
Survival analysis revealed patients with highly expressed CCR7 are subject to a more undesirable prognosis compared with those who expressed low CCR7. Findings of this study coincide with those of other studies [7]. In view of all the evidences, there is reason to believe that the CCR7-CCL21 axis is a crucial cistron in tumor lymph node metastasis. Moreover, as staining for CXCL12 and CCL21 (or CXCR4 and CCR7) was tightly linked in the grouping of primary tumors and lymph node metastasis tumors in this study, it is likely that a shared machinery may account for variations in expression levels of both molecules in breast cancer. Coinciding with previous studies, information technology was demonstrated that levels of combined CCR7 and CXCR4 expression significantly correlated with lymph node metastatic condition[sixteen, 17, 30].
Contempo studies and analyses conducted in the nowadays study clearly point that EGFR expression serves equally the strong prognostic factor in invasive breast cancer [23, 31, 32]. In this study, it was observed that patients with high EGFR expression are more than decumbent to developing metastasis and possessing high grades of tumor, which are both of import prognostic factors for breast cancer patients. Through survival assay, it has been discovered that patients who highly express EGFR are subject to poor prognoses compared with those with low EGFR expression. Contempo reports farther suggest that CXCR4 expression can exist upwards-regulated past HER-2/neu, which is required for HER2-mediated invasion in vitro and lung metastases in vivo [33]. Moreover, the result of the correlation between CXCR4, CCR7, EGFR, and HER-2/neu illustrates that the expression of chemokine receptors (CXCR4 and CCR7) is tightly associated with growth factors (EGFR and HER-ii/neu). Based on this finding, it may be inferred that regulating growth factors may influence the expression of chemokine receptors, which may be helpful in identifying new pathways in breast cancer therapy.
This report was based on a small group of patients. However, it examined corresponding lymph nodes of each patient, and this has not been reported by other scholars to engagement. Although immunochemistry detection of the biomarkers may have certain limitations, it is a elementary and widely utilized technique which can be carried out on routine paraffin-embedded tissues. By contrast, majority of new biological methods require specialized platforms and expertise that are considered impractical in routine pathological diagnosis.
Conclusion
By examining the expression of chemokines and their receptors in both primary tumors and corresponding lymph node metastasis tumors, information indicate that chemokines and their receptors are differentially expressed in the principal and metastatic sites of breast cancer. Results reveal the significant association of CXCR4, CCR7, and EGFR with metastasis and poor prognosis. Farther, the correlation betwixt chemokine receptors and growth factors may provide a new method of agreement breast cancer metastasis and therapy, which are worthy of further study.
References
-
Hassan S, Baccarelli A, Salvucci O, Basik M: Plasma stromal cell derived cistron-i: host derived marker predictive of distant metastasis in breast cancer. Clin Cancer Res. 2008, fourteen: 446-454. ten.1158/1078-0432.CCR-07-1189.
-
Müller A, Homey B, Soto H, Ge N, Catron D, Buchanan ME, McClanahan T, Murphy E, Yuan W, Wagner SN, Barrera JL, Mohar A, Verástegui E, Zlotnik A: Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001, 410: 50-56. 10.1038/35065016.
-
Paget Due south: The distribution of secondary growths in cancer of the breast. Cancer Metastasis Rev. 1989, viii: 98-101.
-
Hassan S, Ferrario C, Saragovi U, Quenneville L, Gaboury Fifty, Baccarelli A, Salvucci O, Basik Grand: The influence of tumor-host interactions in the stromal prison cell-derived gene-1/CXCR4 ligand/receptor axis in determining metastatic take chances in breast cancer. Am J Pathol. 2009, 175: 66-73. 10.2353/ajpath.2009.080948.
-
Cabioglu N, Gong Y, Islam R, Broglio KR, Sneige N, Sahin A, Gonzalez-Angulo AM, Morandi P, Bucana C, Hortobagyi GN, Cristofanilli Thou: Expression of growth factor and chemokine receptors: new insights in the biological science of inflammatory breast cancer. Ann Oncol. 2007, eighteen: 1021-1029. 10.1093/annonc/mdm060.
-
Cabioglu N, Sahin AA, Morandi P, Meric-Bernstam F, Islam R, Lin HY, Bucana CD, Gonzalez-Angulo AM, Hortobagyi GN, Cristofanilli Grand: Chemokine receptors in advanced chest cancer: differential expression in metastatic disease sites with diagnostic and therapeutic implications. Ann Oncol. 2009, xx: 1013-1019. 10.1093/annonc/mdn740.
-
Mattern J, Koanagi R, Volm Thou: Association of vascular endothelium growth factor expression with intratumoral microvessel density and tumor cell proliferation in human being epidermoid lung cancer. Br J Cancer. 1996, 73: 931-934.
-
Zlotnik A: Chemokines and cancer. Int J Cancer. 2006, 119: 2026-2029. 10.1002/ijc.22024.
-
Feng LY, Ou ZL, Wu FY, Shen ZZ, Shao ZM: Involvement of a novel chemokine decoy receptor CCX-CKR in chest cancer growth, metastasis and patient survival. Clin Cancer Res. 2009, 15: 2962-2970. 10.1158/1078-0432.CCR-08-2495.
-
Wang J, Seethala RR, Zhang Q, Gooding West, van Waes C, Hasegawa H, Ferris RL: Autocrine and paracrine chemokine receptor 7 activation in head and neck cancer: implications for therapy. J Natl Cancer Inst. 2008, 100: 502-512. 10.1093/jnci/djn059.
-
Na IK, Scheibenbogen C, Adam C, Stroux A, Ghadjar P, Thiel E, Keilholz U, Coupland SE: Nuclear expression of CXCR4 in tumor cells of non-pocket-size prison cell lung cancer is correlated with lymph node metastasis. Hum Pathol. 2008, 39: 1751-1755. 10.1016/j.humpath.2008.04.017.
-
Hu J, Deng X, Bian X, Li G, Tong Y, Li Y, Wang Q, Xin R, He X, Zhou M, Xie P, Li Y, Wang JM, Cao Y: The expression of functional chemokine receptor CXCR4 is associated with the metastatic potential of human nasopharyngeal carcinoma. Clin Cancer Res. 2005, eleven: 4658-4665. 10.1158/1078-0432.CCR-04-1798.
-
Yoshitake Northward, Fukui H, Yamagishi H, Sekikawa A, Fujii S, Tomita S, Ichikawa 1000, Imura J, Hiraishi H, Fujimori T: Expression of SDF-1 alpha and nuclear CXCR4 predicts lymph node metastasis in colorectal cancer. Br J Cancer. 2008, 98: 1682-1689. 10.1038/sj.bjc.6604363.
-
Gockel I, Schimanski CC, Heinrich C, Wehler T, Frerichs Grand, Drescher D, von Langsdorff C, Domeyer Thousand, Biesterfeld South, Galle PR, Junginger T, Moehler G: Expression of chemokine receptor CXCR4 in esophageal squamous prison cell and adenocarcinoma. BMC Cancer. 2006, 6: 290-296. 10.1186/1471-2407-6-290.
-
Takanami I: Overexpression of CCR7 mRNA in nonsmall cell lung cancer: correlation with lymph node metastasis. Int J Cancer. 2003, 105: 186-189. 10.1002/ijc.11063.
-
Cabioglu N, Yazici MS, Arun B, Broglio KR, Hortobagyi GN, Cost JE, Sahin A: CCR7 and CXCR4 as novel biomarkers predicting axillary lymph node metastasis in T1 chest cancer. Clin Cancer Res. 2005, 11: 5686-5693. 10.1158/1078-0432.CCR-05-0014.
-
Arigami T, Natsugoe South, Uenosono Y, Yanagita S, Arima H, Hirata M, Ishigami S, Aikou T: CCR7 and CXCR4 expression predicts lymph node status including micrometastasis in gastric cancer. Int J Oncol. 2009, 35: 19-24. 10.3892/ijo_00000308.
-
Akishima-Fukasawa Y, Nakanishi Y, Ino Y, Moriya Y, Kanai Y, Hirohashi South: Prognostic significance of CXCL12 expression in patients with colorectal carcinoma. Am J Clin Pathol. 2009, 132: 202-210. ten.1309/AJCPK35VZJEWCUTL.
-
Ding Y, Shimada Y, Maeda M, Kawabe A, Kaganoi J, Komoto I, Hashimoto Y, Miyake M, Hashida H, Imamura Thousand: Association of CC chemokine receptor seven with lymph node metastasis of esophageal squamous cell carcinoma. Clin Cancer Res. 2003, 9: 3406-3412.
-
Sancho G, Vieira JM, Casalou C, Mesquita Thou, Pereira T, Cavaco BM, Dias S, Leite V: Expression and function of the chemokine receptor CCR7 in thyroid carcinomas. J Endocrinol. 2006, 191: 229-238. 10.1677/joe.1.06688.
-
Kato M, Kitayama J, Kazama Southward, Nagawa H: Expression blueprint of CXC chemokine receptor-4 is correlated with lymph node metastasis in man invasive ductal carcinoma. Breast Cancer Res. 2003, five: R144-R150. 10.1186/bcr627.
-
Su YC, Wu MT, Huang CJ, Hou MF, Yang SF, Chai CY: Expression of CXCR4 is associated with axillary lymph node condition in patients with early on breast cancer. Chest. 2006, fifteen: 533-539. 10.1016/j.breast.2005.08.034.
-
Blot East, Laberge-Le Couteulx S, Jamali H, Cornic M, Guillemet C, Duval C, Hellot MF, Pille JY, Picquenot JM, Veyret C: CXCR4 membrane expression in node-negative breast cancer. Breast J. 2008, 14: 268-274. 10.1111/j.1524-4741.2008.00573.x.
-
Salvucci O, Bouchard A, Baccarelli A, Deschênes J, Sauter Grand, Simon R, Bianchi R, Basik One thousand: The role of CXCR4 receptor expression in breast cancer: a large tissue microarray report. Breast Cancer Res Treat. 2006, 97: 275-283. 10.1007/s10549-005-9121-viii.
-
Yasuoka H, Tsujimoto K, Yoshidome M, Nakahara G, Kodama R, Sanke T, Nakamura Y: Cytoplasmic CXCR4 expression in breast cancer: induction past nitric oxide and correlation with lymph node metastasis and poor prognosis. BMC Cancer. 2008, 8: 340-349. x.1186/1471-2407-8-340.
-
Woo SU, Bae JW, Kim CH, Lee JB, Koo BW: A significant correlation between nuclear CXCR4 expression and axillary lymph node metastasis in hormonal receptor negative chest cancer. Ann Surg Oncol. 2007, 15: 281-285. ten.1245/s10434-007-9595-1.
-
Tarasova NI, Stauber RH, Michejda CJ: Spontaneous and ligandinduced trafficking of CXC-chemokine receptor 4. J Biol Chem. 1998, 273: 15883-15886. ten.1074/jbc.273.26.15883.
-
Spano JP, Andre F, Morat L, Sabatier Fifty, Besse B, Combadiere C, Deterre P, Martin A, Azorin J, Valeyre D, Khayat D, Le Chevalier T, Soria JC: Chemokine receptor CXCR4 and early-stage not-pocket-sized cell lung cancer: design of expression and correlation with outcome. Ann Oncol. 2004, xv: 613-617. 10.1093/annonc/mdh136.
-
Gunn MD, Kyuwa Due south, Tam C, Kakiuchi T, Matsuzawa A, Williams LT, Nakano H: Mice lacking expression of secondary lymphoid organ chemokine take defects in lymphocyte homing and dendritic cell localization. J Exp Med. 1999, 189: 451-460. 10.1084/jem.189.3.451.
-
Kodama J, Hasengaowa , Kusumoto T, Seki N, Matsuo T, Ojima Y, Nakamura G, Hongo A, Hiramatsu Y: Association of CXCR4 and CCR7 chemokine receptor expression and lymph node metastasis in human cervical cancer. Ann Oncol. 2007, 18: 70-76. 10.1093/annonc/mdl342.
-
Singh S, Singh UP, Grizzle WE, Lillard JW: CXCL12-CXCR4 interactions modulate prostate cancer cell migration, metalloproteinase expression and invasion. Lab Invest. 2004, 84: 1666-1676. 10.1038/labinvest.3700181.
-
Buchholz TA, Tu X, Ang KK, Esteva FJ, Kuerer HM, Pusztai L, Cristofanilli M, Singletary SE, Hortobagyi GN, Sahin AA: Epidermal growth cistron receptor expression correlates with poor survival in patients who have breast carcinoma treated with doxorubicin-based neoadjuvant chemotherapy. Cancer. 2005, 104: 676-681. ten.1002/cncr.21217.
-
Li YM, Pan Y, Wei Y, Cheng X, Zhou BP, Tan M, Zhou X, Xia W, Hortobagyi GN, Yu D, Hung MC: Upregulation of CXCR4 is essential for HER2 mediated tumor metastasis. Cancer Prison cell. 2004, 6: 459-469. 10.1016/j.ccr.2004.09.027.
Acknowledgements
The work was supported by grants from the Tianjin Natural Scientific discipline Foundation (Nos.06YFJMJC08000 and 09ZCZDSF04400), every bit well as a grant from a key project of the Natural Science Foundation of People's republic of china (No.30830049). Materials were obtained from the Department of Pathology of Tianjin Medical University's General Hospital.
Writer data
Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
Earlier submission, all authors read and approved the concluding manuscript. Amongst the authors, LYX designed the report, while JR collected the materials, performed all experiments, and drafted the manuscript. LJY conducted the statistical analysis and GQ accomplished construction of tissue microarray blocks. ZXL participated in the teaching of the experiment, while ST revised the manuscript critically to ensure important intellectual content. WJJ and LYX read and reviewed the sections, while, LJB and DQY performed follow-up observations on all patients. SBC provided the report concept and participated in its pattern and coordination.
Yixin Liu, Ru Ji contributed equally to this work.
Authors' original submitted files for images
Rights and permissions
Open Access This article is published nether license to BioMed Key Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/past/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and Permissions
Virtually this article
Cite this commodity
Liu, Y., Ji, R., Li, J. et al. Correlation upshot of EGFR and CXCR4 and CCR7 chemokine receptors in predicting chest cancer metastasis and prognosis. J Exp Clin Cancer Res 29, 16 (2010). https://doi.org/ten.1186/1756-9966-29-16
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/1756-9966-29-16
Keywords
- Chest Cancer
- Epidermal Growth Factor Receptor
- Epidermal Growth Factor Receptor Expression
- CXCR4 Expression
- Breast Cancer Metastasis
Source: https://jeccr.biomedcentral.com/articles/10.1186/1756-9966-29-16
0 Response to "Involvement of Chemokine Receptors in Breast Cancer Metastasis Review"
Post a Comment